NEW YORK (Reuters Health) – During thyroidectomy, the technique used to identify the all-important recurrent laryngeal nerve (RLN) matters when it comes to the chances of paralysis of the nerve and hypoparathyroidism – the two most serious postoperative complications of thyroidectomy.
Results of a prospective study suggest that the superior-inferior approach to RLN identification is associated with significantly lower rates of RLN paralysis and hypoparathyroidism compared with an inferior-superior approach to identifying this nerve.
Dr. Bayram Veyseller from Bezmialem Vakif University, Istanbul, Turkey, and colleagues report their findings in a paper in Archives of Otolaryngology – Head and Neck Surgery, available online now.
“In our clinic, we have accomplished over 1,000 thyroid surgeries over the last 10 years. In our experience, we have observed fewer complications with superior nerve identification technique, which led us conduct a prospective study design. Our intention was to share our experience with colleagues,” Dr. Veyseller noted in an email to Reuters Health.
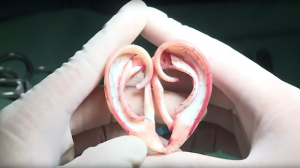
The RLN runs immediately posterior to the thyroid gland and supplies motor function and sensation to the larynx. Because of its close proximity to the thyroid gland, the RLN needs to be identified in patients undergoing total thyroidectomies performed using an extracapsular approach.
The superior-inferior approach identifies the RLN where it penetrates the larynx, followed by superior pedicle ligation, while the inferior-superior approach locates the nerve in the tracheoesophageal groove, and traces it in the superior direction.
Dr. Veyseller and colleagues compared the two techniques in 195 consecutive patients who underwent thyroidectomy for goiter between January 2006 and August 2009 and were followed for an average of 26 months after surgery.
The superior-inferior RLN identification technique was used in 67 of the patients and the inferior-superior method in 128, according to the attending surgeon’s preference.
Their focus was on the incidence of complications, mainly RLN damage and hypoparathyroidism, which occurred significantly less often with the superior-inferior approach (P < 0.05).
No patient in the superior-inferior group experienced recurrent laryngeal nerve paralysis, whereas 2 patients (1.5%) in the inferior-superior group developed permanent RLN paralysis. One of these patients had been admitted with recurrent disease, they authors note.
Four patients (8.3%) in the superior-inferior group developed temporary hypoparathyroidism compared with 14 patients (16.2%) in the inferior-superior group. Four patients (4.6%) in the inferior-superior group had permanent hypoparathyroidism.
The clinicians note in their paper that searching for the RLN in the tracheoesophageal groove and following it where it enters the larynx (the inferior-superior approach) “requires more dissection and can lead to parathyroid devascularization, which can cause ischemia and necrosis and lead to hypoparathyroidism.”
The superior-inferior approach to the RLN, on the other hand, “allows the surgeon reach to the region directly and involves less dissection and less parathyroid damage,” they say.
“This technique,” Dr. Veyseller commented, “entails nerve identification at level of insertion to larynx, therefore requires knowledge of detailed head and neck anatomy and experience with thyroid surgery. We believe, at experienced hands, this approach will result in reduced complication rates.”
The clinicians would like to see their results corroborated with larger case series.
Arch Otolaryngol Head Neck Surg 2011.