NEW YORK (Reuters Health) – Primary total hip arthroplasty with a porous-coated cementless acetabular component continues to provide “durable fixation at 20 years postoperatively,” orthopedic surgeons from Rush University Medical Center in Chicago report.
“Our results confirm earlier work done at Rush and at other institutions that cementless acetabular components work very well and that long-term biological fixation can be obtained,” Dr. Craig Della Valle noted in a prepared statement.
He and his colleagues previously reported the 7- and 15-year results of the use of a porous-coated acetabular metal shell inserted without cement in a consecutive series of 204 primary total hip arthroplasties.
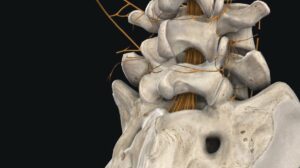
Now, in the May issue of the Journal of Bone and Joint Surgery, they report the longer-term outcomes of these arthroplasties at a minimum of 20 years after surgery. According to the report, 114 (92%) of the 124 hips available for study had retained the original acetabular metal shell.
“The 20-year rate of survival of the metal shell, with failure defined as revision because of loosening or radiographic evidence of loosening, was 96%,” the team reports.
Since the previous report at 15 years, a total of five acetabular components required revision for aseptic loosening or had radiographic evidence of definite loosening, they note.
“Fourteen hips with well-fixed acetabular shells required a change of the modular acetabular liner because of excessive wear and/or for the treatment of osteolysis, and liner changes have been recommended for another eight hips,” they also report.
In a statement, co-investigator Dr. Jorge O. Galante noted that “the high rate of wear-related complications was not completely unexpected,” given that the average age of the patients in the study was 52 years, “much younger than most patients who underwent hip replacements at the time.”
“With time, the number of repeat surgeries due to wear and osteolysis has increased, as have the numbers of cases of osteolysis we identified radiologically,” Dr. Della Valle added. “But with the newer, more wear-resistant bearing surfaces we are now using, we believe that fewer patients today will need revision surgery for these reasons.”
Reference:
J Bone Joint Surg Am 2009;91:1130-1135.